What is a Do Not Resuscitate (DNR) order?
A Do Not Resuscitate order is a legal document that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac arrest or respiratory failure. This order is designed to respect the individual’s preferences regarding end-of-life care and should be discussed with healthcare providers and loved ones.
Who can request a DNR order?
Typically, a DNR order can be requested by a patient, their legal guardian, or a healthcare proxy. In some cases, the healthcare provider may also initiate the discussion, especially if a patient is critically ill and not likely to benefit from resuscitation efforts.
Do I need a DNR order to refuse resuscitation?
No, you do not necessarily need a DNR order to refuse resuscitation. A patient can verbally express their wishes about resuscitation. However, having a written DNR order is beneficial, as it provides clear guidance to emergency medical personnel and healthcare providers in critical situations.
How does a DNR order differ from advance directives?
A DNR order specifically pertains to resuscitation efforts, whereas advance directives cover a broader scope of medical treatment preferences. Advance directives might include decisions about other life-sustaining treatments, like mechanical ventilation or feeding tubes, in addition to resuscitation preferences.
Will a DNR order affect my other medical treatments?
No, having a DNR order in place does not affect the quality of other medical treatments you receive. Healthcare providers will continue to offer all necessary care, except for resuscitation. It is important to clarify your wishes about other treatments in your advance directives if you have specific concerns.
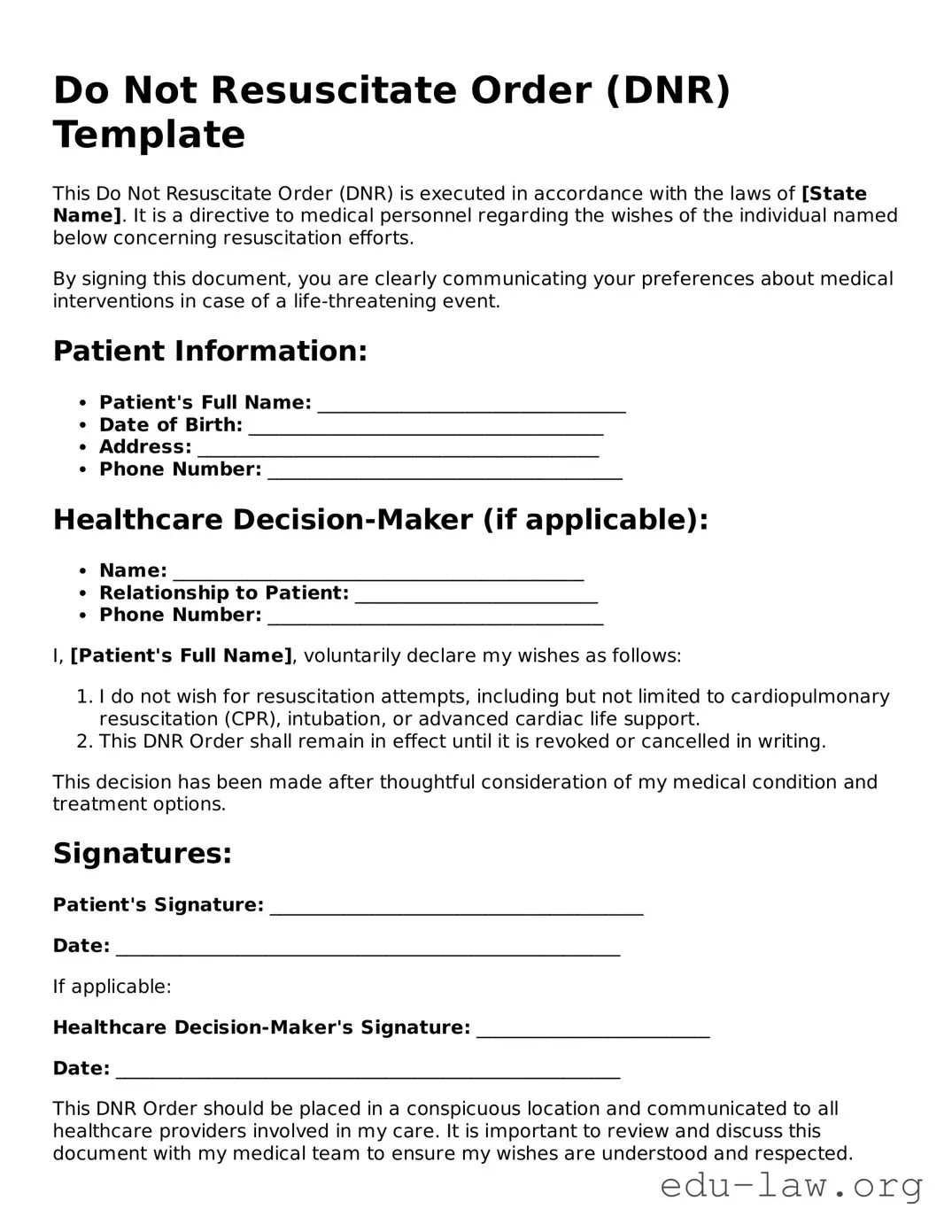
How can I obtain a DNR order?
You can obtain a DNR order through your healthcare provider. They will typically provide you with a specific form to fill out. You may need to have a conversation about your medical condition and treatment wishes, ensuring you fully understand what a DNR means for your care.
Can a DNR order be revoked?
Yes, you can revoke a DNR order at any time. If you change your mind about resuscitation, simply inform your healthcare provider, and they can help you with the process. It is important to communicate any changes to family members and ensure that your new wishes are documented properly.