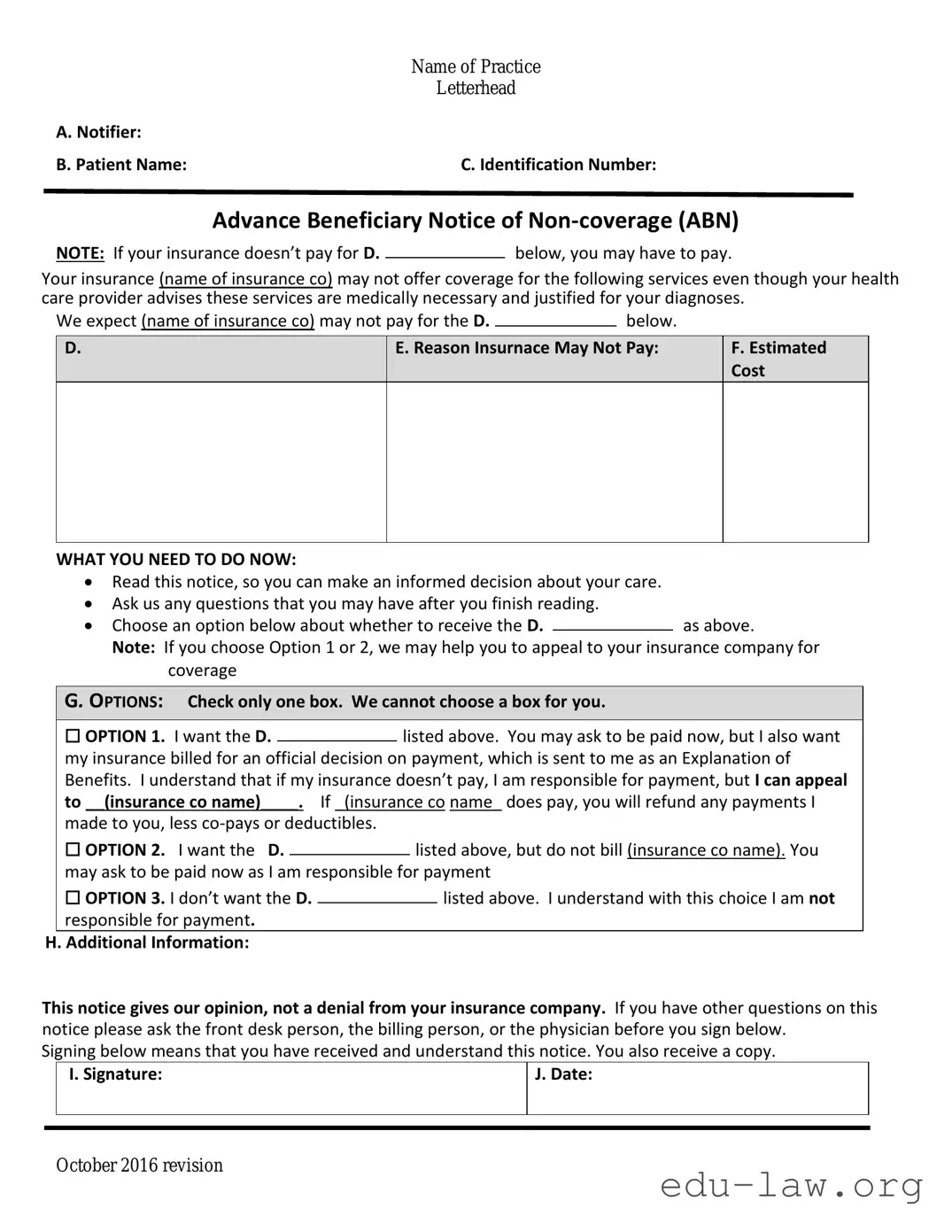
The Medicare Part A and Part B Claim form, known as the CMS-1500, serves a crucial role in the medical billing process. Similar to the Advance Beneficiary Notice of Non-coverage (ABN), this form informs beneficiaries about the services provided and any potential coverage issues. Providers submit the CMS-1500 to request payment from Medicare for services rendered. In both documents, transparency is vital, as they both alert patients to the possibility of denied claims, thereby ensuring that patients understand their financial responsibilities ahead of time.
The Medicaid Patient Confirms Eligibility form is another document that has a relationship with the ABN. This form enables healthcare providers to verify a patient’s eligibility for Medicaid services before providing care. Just as the ABN gives patients foresight into possible non-coverage situations, the Medicaid form assists beneficiaries by confirming whether they will receive financial support from Medicaid. Awareness about one’s benefits is crucial in both scenarios, preserving the patient’s right to be informed prior to receiving treatment.
The Notice of Privacy Practices (NPP) aligns with the ABN in its fundamental objective of informing patients. Specifically, the NPP educates patients about their rights regarding protected health information, allowing them to understand how their data will be used and disclosed. While the ABN focuses on service coverage and associated costs, both documents emphasize the importance of informed consent and patient autonomy, ensuring patients can make educated healthcare decisions.
Another comparable document is the Medical Necessity Documentation form, which is vital for justifying medical services. This form provides evidence that a patient’s treatment aligns with accepted medical practices and is necessary for their health. Like the ABN, this document helps manage patient expectations regarding coverage, as it articulates why certain procedures are deemed medically necessary or not, impacting potential out-of-pocket costs for the patient.
Informed Consent forms also share similarities with the ABN in terms of patient awareness. Informed Consent ensures patients understand the risks and benefits of a treatment or procedure before agreeing to it. While the ABN advises on potential non-coverage for some services, Informed Consent empowers patients by outlining what to expect in terms of care, thereby enhancing patient understanding and agency in their medical decisions.
The Waiver of Liability form serves a similar purpose to the ABN by protecting the patient from unexpected liability. This document is used when a provider believes that Medicare might deny a service but the patient still wishes to receive it. Through the Waiver of Liability, patients can acknowledge their understanding of the potential denial and agree to take responsibility for payment should it occur, akin to the framework established by the ABN where patients are informed of non-coverage possibilities.
The Assignment of Benefits form connects to the themes in the ABN concerning patient rights and financial transparency. This document allows patients to transfer their right to receive Medicare benefits directly to their healthcare providers, which can streamline payment processes. Both forms emphasize clear communication on financial implications, helping patients recognize their responsibilities and rights within the healthcare framework.
Lastly, the Explanation of Benefits (EOB) document elucidates coverage decisions made by insurance providers after a claim has been processed. Like the ABN, the EOB informs patients about what services were covered, denied, or partially reimbursed. This document serves as a critical tool for patients to understand their financial obligations post-service, similar to how the ABN preempts potential billing issues by informing patients before a service is rendered.